The appointment of a physician, Dr. Ben Carson, to run the U.S. Department of Housing and Urban Development (HUD) raised eyebrows. What does a brain surgeon know about affordable housing? But health and housing are intimately linked. Where we live not only dictates our access to opportunities such as education and employment. It shapes our thoughts about what opportunities exist and if they are attainable. It controls opportunities we are exposed to – job or gang. If Dr. Carson reduces segregation by enforcing the new federal fair housing rule, he can advance health equity — the opportunity for everyone to live their healthiest possible life.
During his recent Senate confirmation hearing, Dr. Carson reinforced his position that government should have a more limited role in the provision of housing and noted his own background as a medical doctor as shaping how he would lead the department. What could this mean for Houston?
A day before the Carson hearing, on January 11, the federal government issued a scathing letter outlining in detail a finding that Houston has made decisions about the location of low-income housing in a “racially-motivated” manner, singling out Mayor Turner’s recent decision not to back a housing development on Fountain View in the Galleria area.
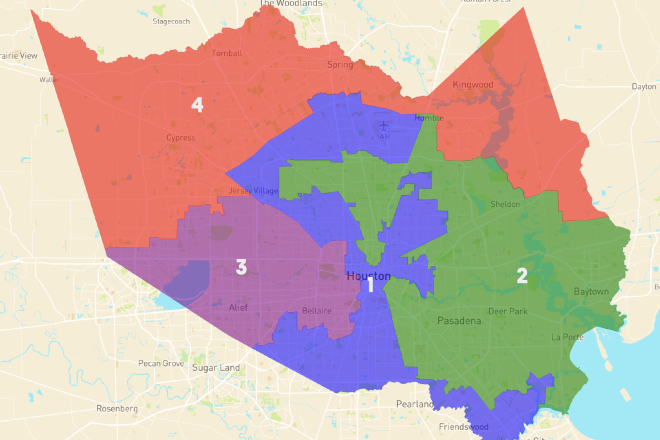
However, the history behind this controversy is long. Susan Roger’s recent article for OffCite about “redlining” is a good place to start. For generations, many hardworking Houstonians were shut out of neighborhoods with the best schools, parks, and jobs. Policies such as the Federal-Aid Highway Act of 1956 and race-based deed restrictions facilitated segregation. Highways, factories, and landfills were concentrated in Houston’s African-American and Latino neighborhoods, as was low-income housing. This concentration of low-income housing is clear to see in the map.
When asked explicitly about his position on HUD's new fair housing rule, which prohibits the concentration of subsidized housing in low-income neighborhoods, Dr. Carson indirectly responded by noting he would work with local communities to make sure “fairness is carried out.” Given the lens through which he intends to promulgate housing policy, it is imperative that we all understand that implementing and enforcing the reduction of residential segregation is also powerful health policy.
Residential segregation is consistently cited as a fundamental cause of racial differences in health. The communities in which we live shape our opportunities for good health, particularly for those with low incomes. Research indicates that an individual’s zip code is a stronger predictor than their genetic code of how long they will live. While health insurance and healthcare access are critical for treatment of ailments, good health starts in the places where we live, work, learn, and play. Good schools, transportation, employment with a living wage, strong social support networks, safe housing, and public safety have more to do with our health outcomes than health care.
One indicator that illustrates this difference is life expectancy by race and income. A recent analysis found that nationally, there is a 15-year difference in life expectancy between men in the top 1 percent of income compared with those in the bottom 1 percent – and the gap is growing. There is an almost five-year difference in life expectancy for black and white males. However, national trends obscure vast differences in health at the community level where health is produced. According to research funded by the Robert Wood Johnson Foundation), in New Orleans, there is a 25-year gap in life expectancy between communities just a few miles apart.
Although the Fair Housing Act of 1968 outlawed housing discrimination, segregated housing patterns persist. Residents mount vehement resistance when attempts are made to integrate affordable housing into neighborhoods which have been afforded more opportunities. Excluding people from places rich with opportunity, or refusing to invest in neighborhoods that have been left behind economically, cripples our efforts to achieve health equity.
And we all bear the costs from the health inequities that ensue, in part, from residential segregation. According to one estimate, between 2003 and 2006, health inequities cost our nation $1.24 trillion for both direct medical care and indirect costs.
During his testimony, Dr. Carson acknowledged the intersection between housing and health. However, he fell short of clearly articulating his support for reducing residential segregation, or how he would work collaboratively with other agencies to improve low opportunity environments for HUD beneficiaries.
Remarkable individuals like Dr. Ben Carson manage to escape low opportunity, but research indicates that 70 percent of those who grow up poor will remain poor for the rest of their lives. And, even when individuals are able to move out of poverty, growing up poor compromises their health as an adult, increasing the likelihood of developing mental health problems and other chronic illnesses.
Our ability to move the needle toward health equity is at great risk if Dr. Carson does little to enforce the new fair housing rule. Low-income people, especially those of color, simply cannot afford to rely solely on compassion and goodwill to improve the places where they live.
Given the association between poor health and residential segregation, Dr. Carson is obligated to vigorously enforce the new fair housing rule – not only because of his position as HUD Secretary but also because of his obligation as a physician to do no harm.
Dr. Nelson received her doctorate in Public Policy from the University of Maryland, Baltimore County and is founder of Community Health Collaborative Consulting. See her talk for the Rice Design Alliance civic forum on walking and health in Harris County.